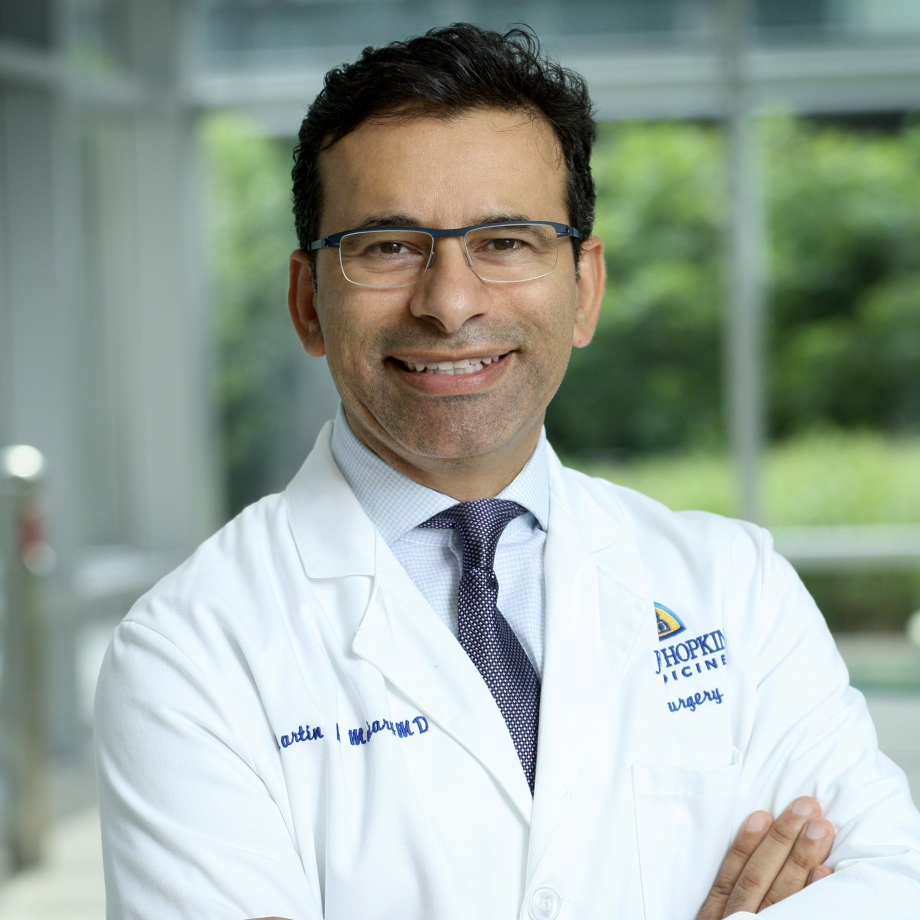
Dr Marty Makary is a New York times bestselling author, Johns Hopkins gastrointestinal surgeon and professor of health policy. His newest book, The Price We Pay, is out this week and has been called the big short of American medicine. Marty’s research has led to actionable solutions that reduce waste and over treatment, improving the quality of care to the patient and saving our healthcare system millions of dollars. As you probably know, his previous book, Unaccountable is now a hit TV series. You want to stay tuned to hear his thoughts on what he calls the crisis of appropriateness. And now please join me and our guest for a second opinion.
Marty Macquarie, a surgeon first and foremost, a journalist, a author, public policy expert, a professor of health policy at Johns Hopkins. You’ve really done it all, which I really admire you for, which is really unbelievable and we’ll come to that. I think there are a number of things I want to come to, but I think the titles of your last two books, one of which is right here, kind of tell the story and the topics that we ought to spend the next few minutes talking about. And then there’ll be the transparency and accountability but, Unaccountable, a book, a subtitle being, “what hospitals won’t tell you and how transparency could revolutionize healthcare.” It very quickly comes unaccountable transparency. By the way, for our listeners, a great TV medical show, The Resident inspired off of that. And then the other book, the book that I have right here next to me, The Price We Pay. And then the subtitle, which I think really tells the whole story is, “what broke American healthcare and how to fix it”, which we’ll come back to. So welcome. Thanks for being with us.

Marty Makary: Great to be here with you.
Bill Frist: Let’s forget all that though for a second and and come to something that’s common to you and that is being a physician and you’re involved in policy and you’re involved a lot in communication of what we have done, but really more what should be done. Being a doctor, how has that colored, what doors has it opened? What has it allowed you to do taking that Hippocratic oath going through medical school and training?
Marty Makary: Well, I think it’s a great privilege for us to be in a profession that has such an incredible history. And if you look at Hippocrates, Benjamin Rush, Dr Sabin, curing polio, some of these modern heroes and folks out in Africa doing incredible work, it’s an incredible profession to be a part of. And when somebody comes up to you in the emergency room and trusts you to put a knife to their skin within two seconds of meeting you, just because you’re the doc or they’ll tell you a secrets they’ve never told their spouse, it’s this incredible privilege. And I think with that comes a certain sense of responsibility to uphold the nobility and the altruism of our profession. So I love it. I feel like it provides some credibility.
Marty Makary: I think that all of my research ideas come from either operating and managing patients and working in the clinic, or they come from the docs that I get to meet on the road and we both get the privilege of talking to so many doctors around America. That’s where all the good ideas are. And so it’s been great. It’s been a great run. I love being a doc and I love being able to advocate for patients. My dad was a cancer doctor.
Bill Frist: Was he? Yeah.
Marty Makary: And he always felt like when you have cancer, you’re vulnerable and you’re scared. And it was his responsibility he felt to advocate for them to make sure they could get their immune therapy or their plasmapheresis at whatever time in the middle of the night because they were not a special interests. They’re not a lobby. Patients are really a part of the herd that we’re called to shepherd.
Bill Frist: Do you think that sort of intimacy of the relationship and the trust where that you come back to again and again in your speaking and your talking and in your writing, does all of that lead you to have most of your conversations and writings and speeches to doctors or to patients? And are you the voice of the patient and your voice or the doctor? Again, you’re all over the place I know, but in your mind are you more a spokesperson identifier with the physician or the patient?
Marty Makary: I would say maybe the physician. I mean, I think that it’s part of our profession and it’s an incredible group of people that are called to this task of advocating for patients. I think though that, you know, people ask sometimes, “Why are you talking about this stuff? Why are you talking about middlemen and price transparency and quality and accountability and healthcare? And aren’t you worried about what other people are going to think of you?” Look, I’m a cancer surgeon. I break bad news. Life is short. I mean, I’m very aware that my time on earth is limited and you got to speak your mind. You got to do what you think is right. Most doctors are trying to do what’s right. Most doctors do the right thing or always try to, and I think if we can rally doctors around the incredible heritage that we have in medicine to really be self-sacrificial and do whatever it takes for the patient, not only is it noble, but it’s the fun part of the job.
Marty Makary: I mean, as a surgeon, that’s what we did in surgery, right? It didn’t matter how long the operation took or if you were paid $1 million to come in at two in the morning morning or you had to pay a million dollars to come in at two, whatever it took to be there for the patient. And it’s really something inspiring. I think ultimately we want to be, everyone in the world wants to be a part of something great and meaningful and medicine is just a great profession to be a part of. And you know, I was literate in medicine but not literate in healthcare. And as I’ve learned from you and watching you do so many great things in health care, we can also become literate in healthcare. And if we can get doctors to be literate, not just in the practice of medicine but in healthcare, we could be an incredible force.
Bill Frist: Purpose is not to sell your book, although we need to sell your book. But tell us the story of this particular book, which is very current. If there is one issue among the American people that’s shown in polling in Washington DC where I was yesterday, it is the price, it is things are expensive, I can’t afford it. And your book is very much about the price. But tell us the story of what you did to come up to produce this book. What’s behind this book and then what is the fundamental message of the book?
Marty Makary: Well, most Americans, as you and I were talking about earlier, don’t live like you and I. We’ve been blessed. God’s been good to us. We’re doing fun stuff. I don’t even feel like I’m working. I don’t know about you, I mean it’s like we getting to learn and share. And most Americans don’t have $500 of cash on hand. Most Americans, when you go to their house, would love to be somewhere else. Or they live in a high crime neighborhood in Baltimore where I work or they would love to have their kids in a better school. A lot of people are hurting out there. And in this book I wanted to tap into the intense frustration out there about healthcare.
Marty Makary: How do people feel about it? I wanted to talk to healthcare and insurance companies and hospital CEOs and the middle layers and the innovators and the disruptors and the startup companies and the patients. So over the course of two years with the help of an editor who commanded me to get on the ground in each one of 22 cities, I traveled and met with folks. And what I found is what you touched on, people are getting crushed out there. People are frustrated. If a quarter of all Americans are avoiding medical care for fear of their bills or a distrust in the system, it didn’t matter if we cure pancreatic cancer, if we can’t get that cure to the 40,000 Americans that have it because a quarter of them don’t trust us anymore, we’re not going to be effective. So there’s the implementation science is harder than the discovery science sometimes and the translation of what we should be doing to what we’re actually doing to me, that’s the challenge where we can do a lot better.
Bill Frist: Yeah. And let’s talk a little bit more about that. And so the price and the cost or spending, all of which can be lumped together to some extent, let me ask you a couple of questions. Do we spend enough on health care today? 18% of GDP, which again means nothing to most people, but when you take it down to a personal level, it’s about $11,000 a year spent on every single person. Is that too much or too little?
Marty Makary: Too much.
Bill Frist: And if it’s too much, you imply one of three things. We spend too much on administrative costs, which is really increased over the last 20 or 30 years. All sorts of things that are nonmedical delivery or we spend too much overuse or we spend too much underuse like preventative care or there’s just misuse. So how do you address that?
Marty Makary: Both overuse and underuse are big problems, but by far overuse is dominating the healthcare system. Now, mostly because of the perverse incentives that are intrinsic, but we also have a geographic or what I would call a distribution problem. It may not be that we have too many dermatologists. It may be that we have too many dermatologists living in Philadelphia and in Los Angeles. There’s real skin cancer needs out there in West Virginia and so we have a distribution problem as well. It would be a little arrogant of me to say we’re spending too much, but here’s what I can put together.
Marty Makary: Here’s an employer who’s delivering great healthcare to their employees for $4,000 total spend per employee per year on average, one of the big retailers in Texas. Here’s an employer spending $12,000 per year per employee on healthcare and they’re very dissatisfied and their deductibles are very high. Here you have a $300 deductible with a total $4,000 spend and great satisfaction, and here you have intense frustration. There obviously is tremendous waste that’s driving that higher cost and we can do better. We can have more efficient health care. We can listen to the voice of doctors who oftentimes telling me on the road, I don’t know if you’ve heard this, look, I can design health care better, but no one’s really asking me for my opinion. If you wanted to know how to design the whole mental health model of how we take care of people better than the job we’re doing now, I could tell you how to do it. It’s just no one’s been asking me.
Bill Frist: Yeah.
Marty Makary: And so there’s tremendous wisdom that lives in medicine. We just have to tap it.
Bill Frist: And how much waste is there? Commonly the policy makers say there’s 20 to 35% waste in the system. When people ask you that question, since you really studied it, how much waste do you perceive or think or have studied, is there and what can be done about it?
Marty Makary: Sure. So the best analyzes show about 20% administrative waste and doctors when we survey them nationally, say that 21% of all medical care is unnecessary. So 40% of that giant healthcare spend of 3.5 trillion is avoidable and unnecessary. We can do a lot better. We wouldn’t tolerate that in any other industry. So we can take a close look at the low hanging fruit, how health care is sold to businesses in the marketplace.
Marty Makary: Once again, as a surgeon, I love my job. I didn’t know squat about how healthcare is sold to businesses. It’s sold through health insurance brokers. The brokers take a two to 6% commission, sometimes lifetime on every health insurance premium dollar spent. Health insurance companies will then pay the brokers on the backend for getting the business and retaining the business. So the brokers have an intense incentive, they may not follow it and there’s very good people in the broker world who don’t follow those perverse incentives but brokers are incentivized to keep you with the insurance company that’s taking care of them the best.
Marty Makary: So then you get an announcement that your premiums are going up 15% and employer says, “Wait a minute, that’s too much.” And the broker says, “Let me work on this. Okay, I got it down to 9%?” How is it that fluid, right? There’s a tremendous amount of waste. We could sell health care more efficiently. We could get rid of, this is a controversial position, but I’m going to put it out there, get rid of all kickbacks in healthcare, 100%. PBM brokers, the PBMs themselves from the pharma companies, GPOs, let’s make an an honest business and whatever needs to be paid to the middle layer, just put it in the contracts to the end recipient of services.
Bill Frist: Yeah.
Marty Makary: Tremendous amount of money there.
Bill Frist: And now a quick word from our sponsors that make this podcast possible. For 35 years. MEDHOST has been partnering with community hospitals and specialty healthcare facilities that focus on what matters most, effectively taking care of their patients. Trusted by over a thousand health care facilities, MEDHOST offers a full suite of healthcare, IT, and business solutions, including an EHR in emergency department information system. Health care providers need a partner who can help them meet patient needs with agility. Backed by world-class support, MEDHOST Solutions are an ideal match for facilities wanting to enhance patient care. Learn more, go to medhost.com.
Bill Frist: Located in the nation’s healthcare capital, Nashville, Tennessee. Belmont university is preparing the next generation of healthcare leaders. Students in Belmont’s nursing, public health, exercise science, social work, physical therapy, occupational therapy, and pharmacy programs find themselves on the cutting edge of healthcare education featuring an innovative curriculum, comprehensive clinical preparation, and state-of-the-art facilities. For more information, visit belmont.edu\healthcare. And now back to the episode.
Bill Frist: Tell me about your peer to peer letters. There are a number of things that you’re known for nationally, it’s the transparency, it is the waste issues, it’s the overall mission of what healthcare is about. And I do want to come back to the checklist, but also when people say peer to peer letters and when you talk about it, what sort of impact have they had? And give us an example.
Marty Makary: Well, I think doctors are intensely frustrated. You remember this sort of early metrics that were very immature, raw, and unfair to us that measured us as surgeons, your overall mortality rate. I mean you do incredible transplant operations at Vanderbilt, I do pancreatic surgery at Johns Hopkins, we took care of some of the toughest cases, to rate us with an unadjusted mortality rate just created animosity and it alienated a lot of docs. Medicine is an art, as you know. We should tailor treatments to individuals. It shouldn’t be all or nothing. You’re good or bad or this bad event happened and that’s a… We should embrace variation but within a certain boundary and in the letter campaign, what we call the dear doctor letter campaign after NPR did their initial story, the docs love it because one, it’s non-punitive, the data is fed back to them on how they’re doing without them having to voluntarily self-report, which honestly is a burden as well. And it’s not good data. And it’s peer to peer and the docs decided what to measure. They’re showing you where you stand relative to other docs.
Marty Makary: So we’ve seen tremendous leadership from a number of doctor associations to say, “Hey yeah, we want to embrace a measure, a practice pattern measure, not a one case level measure. And we want to share with doctors where they stand around that metric.”
Bill Frist: So what was an example? I’ve forgotten what the initial letter campaign was. I remember reading about it.
Marty Makary: So, skin cancer surgery was one of the projects where the doctor saw how many blocks they used to take out a skin cancer. It should be within a range that they embraced. But the outliers who, I don’t think of them as bad, I think of them as doctors that need help. They saw where they stood and they improve.
Bill Frist: So they were taking too many, they were taking more blocks or several standard deviations more than what’s regarded as the very best.
Marty Makary: Yeah, exactly. They were statistical outliers. And they’re paid by block, the number of blocks.
Bill Frist: So there’s an incentive.
Marty Makary: Yeah.
Bill Frist: So what did you do? So you or somebody wrote a letter to them and did what? Did they get after them and punish them?
Marty Makary: No.
Bill Frist: Or embarrass them? What did the letters say?
Marty Makary: No, these letters were friendly. It’s a look as a courtesy. And it came from the specialty association. They wrote a one-page cover letter and then page two was the data report showing doctors where they stand on the bell curve and the extreme outliers you know, we’re competitive people, docs, right? And school, we don’t like to be outliers. So they self-corrected. Some sought help and I thought, gosh, this is impressive. This is medicine. This is the spirit of collegiality and we can do this without, you know, consultants and big money and regulation and that little program sending letters out to half of the most surgeons in the United States cost 150,000 but saved Medicare $22 million. And I think it shows the spirit of self-improvement. We want to do what’s best for our patients. We want to help our peers. We don’t want to be outliers. And when you appeal to the best in people, they will outperform every time.
Bill Frist: It’s such an important message again for the policy maker. And I think in the conversations that I have in Washington, do you use a carrot or do you use a stick? And really you don’t use either. You don’t have to pay them to do better and you don’t have to just beat them. You just need to make them aware. And people go to medical school with a mission and a lot of people don’t understand that with a mission to help, to lift people up, to heal and are just not aware. And just that lack of awareness, if you make them aware, then they ask the questions and they self correct. Was there any sort of trial if you did use a carrot versus a stick versus the sort of awareness letter of what works and what doesn’t?
Marty Makary: Well, Medicare and the center for Medicare Medicaid services, CMS has been really interested. They did their own project letting doctors know that they were prescribing a ton of Seroquel, which should be prescribed sparingly in older patients. So the high Seroquel prescribers got a nasty letter threatening an audit and the nasty letter verse compared to our friendly letter around most surgery had the same impact. And that is, you don’t have to be nasty, people respond to collegiality. And when it’s a peer to peer doc thing, it can be powerful.
Marty Makary: We’re now doing the same thing and CMS has taken leadership on using this improving wisely model for opioid high prescribers. After a lumpectomy, you shouldn’t be giving women 30 oxycodone.
Bill Frist: Yeah,
Marty Makary: And that we can see in the data who’s doing that in narcotic naive patients regularly. Not a one off, but one woman needs 30 she needs 30 but if you’re doing it on every patient, these are things where we can help each other as physicians. And you know, I love the concept of transparency because it’s an American idea. Matter of fact, the book Unaccountable, I wanted to call it Accountability because it’s a positive idea. But of course the publishers like to, you know, spin things as you know, danger and that and it’s always a challenge managing the messaging.
Bill Frist: But New York Times best seller, spawned off a great television show. So the title might’ve worked. Tell me, so just let me tick off a few things. You’re known as the checklist doctor. Where did that come from? What’s the impact been? Who’s picked up on it? Just elaborate?
Marty Makary: Well Peter Pronovost invented the idea of using a checklist in the ICU to review daily goals and when he started using it for central line placement, that is doing the things we’re supposed to be doing. And we both put in hundreds of central lines. There’s certain things we should be doing but we’re so rushed sometimes. We were just so into getting it done quickly. He protocolized it in a checklist and I started on faculty at Johns Hopkins right when that started. He said, “Marty, for your project, you may want to consider making a checklist for surgery for the operating room.” You’re a surgeon. He was an ICU doctor, and so I put together a checklist. We published it, we piloted the thing at Hopkins in two of the hospitals. It took some real negotiating to get the my colleagues in surgery to use it.
Marty Makary: Initially, they didn’t love the idea. I mean, we’re asked to do a lot of stuff. It was kind of seen as a burden, but then I invited them to be a co-author on a publication, on the checklist on a trial, and then they were very excited to be using the checklist and we got a grant too that helped fund some of this, so they were happy to be a part of a grant, happy to be a part of a publication, and as they used it in the trial, they realized we really like this. The nurses were saying, “No one’s ever asked me for my name in 10 years. I’ve been working with this surgeon, he doesn’t even know my name.” Because we rotate a lot. And it created this great culture where we wanted a culture of speaking up. It’s a safety net for mistakes and things that go wrong.
Marty Makary: And around that time the World Health Organization said, “Hey, we’re forming a committee to talk about surgery and safety. We’ve asked Atul Gawande to head the committee, will you come and present your publications on the checklist?” Well, Atul had his own suggestion, but eventually he fell in love with the idea of a checklist and he’s been terrific and disseminating the concept in the book, The Checklist Manifesto. He’s been a great advocate for it, doing good work right now with his new venture. So that’s the story of the surgery checklist.
Bill Frist: And every operating room now has a checklist and like in the world of aviation that you’re familiar with and I’m familiar with, it has a huge impact for the reasons that you’d said, a huge contribution. A lot of the times you talk about the crisis of appropriateness. What do you mean by that?
Marty Makary: Well, you know, we prescribed as physicians 10 years ago, 2.4 billion prescriptions. Last year it hit almost 5 billion. Did disease double in 10 years.? No, we have a crisis of the medicalization of ordinary life, giving a pill to every condition out there that we can treat oftentimes with lifestyle or good food. It’s hard to watch. And when as healthcare becomes unaffordable for hardworking Americans, you wonder, do we need to be doing all this stuff? I mean, I was talking to spine surgeons who were telling me a lot of that spine surgery can be managed in ways without surgery.
Bill Frist: Yeah.
Marty Makary: And, you know, you listen to docs. Let’s forget about, you know, I might have an opinion about this or that from an experience that I saw. Listen to doctors, they’re saying that we have 21% of all medical care that’s unnecessary, but there hasn’t been funding to look into this. All the funding is skewed towards breast cancer, gene therapy and we could do a much better job funding, what food should we be eating, how can we prevent some of this disease? Should we be giving hormone replacement therapy to post-menopausal women? The trial actually showed it’s safe but was misinterpreted as HRT can cause breast cancer. We should answer that question, that study is old and we still have docs out there saying that it causes breast cancer when it doesn’t. It never did. We can address the actual questions the public is asking.
Bill Frist: And is that more than… And people talk about evidence based medicine, is it an expansion of that or is that a subset of that? Or is it something totally different that we need to be addressing?
Marty Makary: I like the idea of evidence based medicine. We’re wired that way.
Bill Frist: Yeah.
Marty Makary: But can we learn from wisdom? Is there wisdom based medicine? When you have docs saying, “Hey, we should not be doing this.” When you have a whole generation of young nutrition science experts and cardiologists saying, “Hey, saturated fat not cause heart disease. The studies showing it was were bad and look at all the natural reasons and why we believe from the mechanism of action that saturated fats are not bad for you and if we demonize it, we’re going to move the food industry to carbohydrates, which are probably the real trigger of inflammation.” We can probably be more humble as a profession. I try to use my platform at Johns Hopkins a little bit to talk about humility with the younger students, I try to use my position of tenure to talk to the newer faculty members that I mentor about humility. I mean, do we owe the public an apology? Does the American Heart Association owe the public an apology for demonizing fat for 50 years? The HRT study, do we owe the public an apology that we spent a billion on that trial?
Bill Frist: You talk a lot in the book, you opened the book and the theme of the book, very much of the book, The Price We Pay is, and your last sentence I believe or last paragraph talks about restoring medicine to its noble mission. What do you mean by that? Because I think we’re beginning to talk about that, but it is the overriding theme of the book itself. What do you mean by that?
Marty Makary: You know, if you look at the reasons we went into medical school and the reasons kids today want to go into medical school, it’s awesome. They want to make a difference in the world, they want to help people. Talk to a student and in high school that says, “Yeah, I’m thinking about maybe doing nursing.” They’re different from their peers. Even in business, the people that go into managing hospitals, they’re different from their peers. We’re all attracted to this profession out of sense of compassion.
Marty Makary: But then we’re working in such a strange, fragmented, messy system where the alignment of incentives cross and short circuit and it creates these silos and animosity. And we just need to get people back in the room and say, “Let’s remember the reason we went into this profession. It wasn’t to shake people down for every last penny that can’t afford a marked up bill. It wasn’t to recommend a blood test that has no evidence to support it. We went into this to help people,” and I still believe we have the absolute best doctors and hospitals than anywhere else in the world. We’ve had the privilege of working at some of them and it’s inspiring.
Bill Frist: It is, and the medical students coming in, we have more people applying to get into medical school than ever and I know you talk a lot about it. Something happens in that training. They come in, they want to just lift individuals up. They want to heel and they’re willing to kill themselves to do it and the money doesn’t matter at all. I think we all as a profession have a responsibility and as a society to recognize that we can’t keep squeezing through medical school and internship and residency and temptation and payment mechanisms and all. We can’t squeeze that good intention out of those young students because they’re there for a reason. We’ve got to keep that mission well defined for them.
Marty Makary: I agree. We’ve got to preserve all that creativity and drive and compassion instead of beating into them the urea cycle that they got to memorize six times over. I mean we don’t need to have them memorize that urea cycle. You don’t need to… If you’re going to be a cardiac surgeon, you probably don’t need, as you did to spend five years in general surgery managing pancreatic abscesses for you know, in the middle of the night to be a great cardiac surgeon. You might do better… I personally would have benefited from teaching on how to break bad news or hold a meeting, you know? Or the healthcare literacy.
Bill Frist: And the communication skills and the empathy and medical education clearly needs to be modified and it’s moving slowly. But I think that through your writings, through your great work that we can change that culture and the magnetism here, the two books that I mentioned, Unaccountable, again, the bestseller and The Price, which is on its way to be the bestseller, really bring up these current themes today. And you articulate it so well, you put that together. It’s sort of the accountability of the pricing, the dramatic changes and what’s behind it. If you have to really step back and go to 30,000 feet, are you optimistic where we are today and at least the trajectory of where we’re going? Or are you pessimistic and that’s why you’re working so hard and writing more books because you got to get the message out?
Marty Makary: I’m actually deeply inspired by all the innovators and young doctors and senior folks that are saying, “Hey, I’ve been saying this all along.” I am so big right now on healthcare. I’m optimistic. I mean seeing exciting things, I feel like we’ve learned our lesson that the government is not going to fix this for us. And you’re seeing employers redesign care and IOR health and ChenMed come up with a totally patient centered way of doing primary care to fix the broken primary care system and scientists publishing articles showing we’ve been doing too much are indications for doing this procedure have been too broad. Here’s the precise precision medicine approach to fix the subgroup. And if we do appropriate care and can restore some healthy competition and price transparency and quality transparency and they have to go together, we can see a tremendous improvements in healthcare.
Marty Makary: And I think it’s just exciting I get to watch this. I mean watching these startups and innovators and big companies come up with better ways of doing things. Aspire Health, one of them you’ve been involved in, but it’s inspiring, it’s refreshing. And I think my favorite movie was The Big Short. If you’ve seen that.
Bill Frist: Uh-huh.
Marty Makary: And you know, it took a very boring and complex subject, the financial crisis, credit default swaps, collateralized debt obligations, things that are intensely boring and it made it understandable to the everyday person and said, “This is not something only experts can understand. You can understand it. The banks are spending money, they don’t have, it’s your money.” And healthcare is the same thing. There’s a lot of stuff that can be explained to the everyday person. Good RX just did this, the app.
Bill Frist: Yeah.
Marty Makary: Navigating people to the best price for a drug. Forget about all the middlemen and games. If he just walked in without insurance, what would they price it for? And so it’s exciting, don’t you think?
Bill Frist: It’s an exciting time and I share your excitement and I think you capture that. And again, I love the title of the book of The Price We Pay and “what broke American healthcare.” And you did it by traveling to 22 cities, talking to real people as well as the professionals and then the real subtitle of, “and how to fix it.” And we can fix it. It can be done and you outline it so well in the book.
Marty Makary: Thanks.
Bill Frist: Thank you so much again, a conversation that will continue both on the road but back here together and once again with our listeners. Thank you Marty.
Marty Makary: Great to be with you Senator, awesome.
Bill Frist: Thank you, man. Appreciate it. Thanks. This episode of A Second Opinion was produced by Todd Schlosser, Motus Creative Group and Snapshot Interactive. You can subscribe to A Second Opinion on Apple Podcast or wherever you’re listening right now and be sure to rate and review A Second Opinion so we can continue to bring you great content. You can get more information about the show, its guests and sponsors at asecondopinionpodcast.Com, that’s asecondopinionpodcast.com. Thank you again to our sponsors, MEDHOST and Belmont University. Be sure to join us for our next episode where we dive into social determinants, rural maternal health in a wonderfully engaging discussion with Dr. Kara James, Director of the Office of Minority Health at CMS, the Centers for Medicare and Medicaid services. A Second Opinion broadcast from Nashville, Tennessee, the nation’s Silicon Valley of health services where we engage at the intersection of policy, medicine, and innovation.